Applanation Tonometry
Radial or carotid tonometry is performed using a handheld strain gauge pressure sensor over the artery. The pressure in the vessel is transmitted to the sensor and recorded digitally. Using a mathematical formula, central blood pressure is derived and calculated from peripheral blood pressure and concomitant recording of a pulse pressure wave with applanation tonometry.1
Using applanation tonometry to measure central blood pressure can be difficult and time consuming and the results may be operator dependent. A recent study has shown a discrepancy between radial and brachial systolic blood pressure, which highlights inaccurate readings of central systolic blood pressure when brachial-calibrated radial tonometry is used.2

1. da Mota Dias, E, Giollo, LT, Martinelli, DD, Mazeti, C, Júnior, HM, Vilela-Martin, JF & Yugar-Toledo, JC 2012 ‘Carotid Intima-media Thickness Is Associated with Cognitive Deficiency in Hypertensive Patients with Elevated Central Systolic Blood Pressure’, Cardiovasc Ultrasound, vol. 10, no. 41, pp. 1-11. Article
2. Climie, RED, Picone, DS, Keske, MA & Sharman, JE 2015 ‘Brachial-to-radial systolic blood pressure amplification in patients with type 2 diabetes mellitus’, Journal of Human Hypertension, doi:10.1038/jhh.2015.101.
Cuff-based oscillometry
Central blood pressure monitors, such as the Uscom BP+, use Pulse Wave Oscillometric technology.
The theory of wave reflections implies that the pressure at any location in the arterial tree can be considered to be the sum of forward- and backward-going pressure waves. The arteries most relevant to the cuff-based oscillometry measurement technique are shown in the Figure 1.
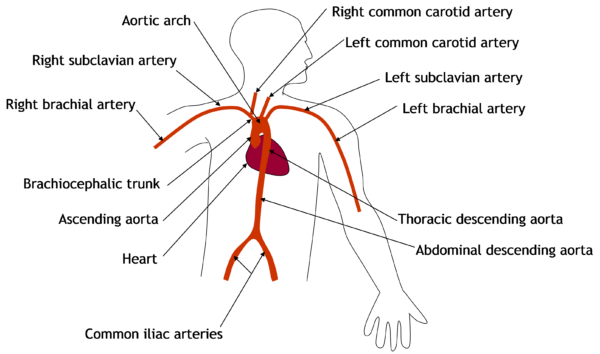
Figure 1: Arteries of the upper body
The initial forward-going pressure wave is generated by the contraction of the heart’s left ventricle. Backward-going pressure waves are created when the forward-going pressure wave encounters a change in the properties and geometry within the arterial system. At such a point, the forward-going wave is partly reflected, creating the backward-going pressure wave. There are multiple reflection sites within the human arterial system.
The cardiovascular monitor is designed to measure pressure-related information from the upper arm using an inflatable cuff. As shown in Figure 2, the pressure wave generated by the heart can be considered to take two paths to the upper arm cuff, generating what are known as the incident wave and reflected wave.
- The incident wave travels from the heart, through the ascending aorta, subclavian artery and brachial artery to reach the cuff.
- The reflected wave travels from the heart, through the ascending aorta, aortic arch and down the descending aorta to the effective reflection site in the abdominal aorta. At this location, some of the forward-going wave is reflected and travels back up the descending aorta, through the subclavian and brachial arteries before arriving at the cuff.
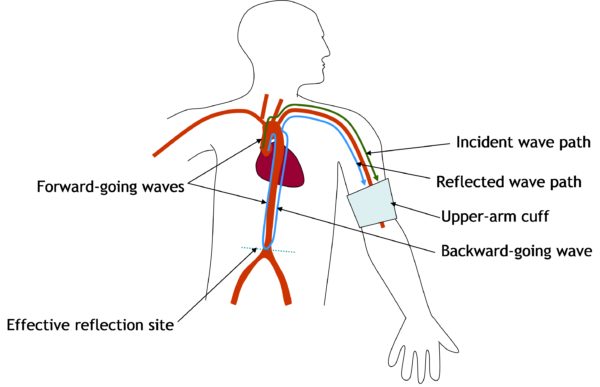
Figure 2: Pressure wave reflection in the arterial system
Measurement should be performed on the left arm. In cases where left-arm measurement is contraindicated, measurement from the right arm can be performed. As with all oscillometric blood pressure measurements due to the additional complexity of the wave path to the right brachial artery, results from the right arm will differ and are not directly comparable with left-arm results.

Figure 3: Central blood pressure cuff
Augmentation Index
The augmentation index is a ratio calculated from the blood pressure waveform, it is a measure of wave reflection and arterial stiffness. Augmentation index is commonly accepted as a measure of the enhancement (augmentation) of central aortic pressure by a reflected pulse wave (shown in green in the graph).
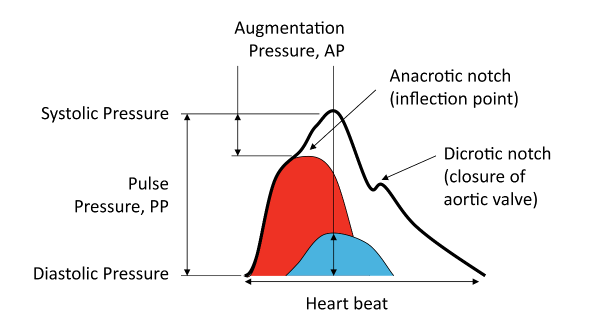
Figure 4: Augmentation Index
More information on central blood pressure:
http://www.dialogues-cvm.org/document/77/DCVM77.pdf
http://eurheartj.oxfordjournals.org/content/ehj/35/26/1719.full.pdf